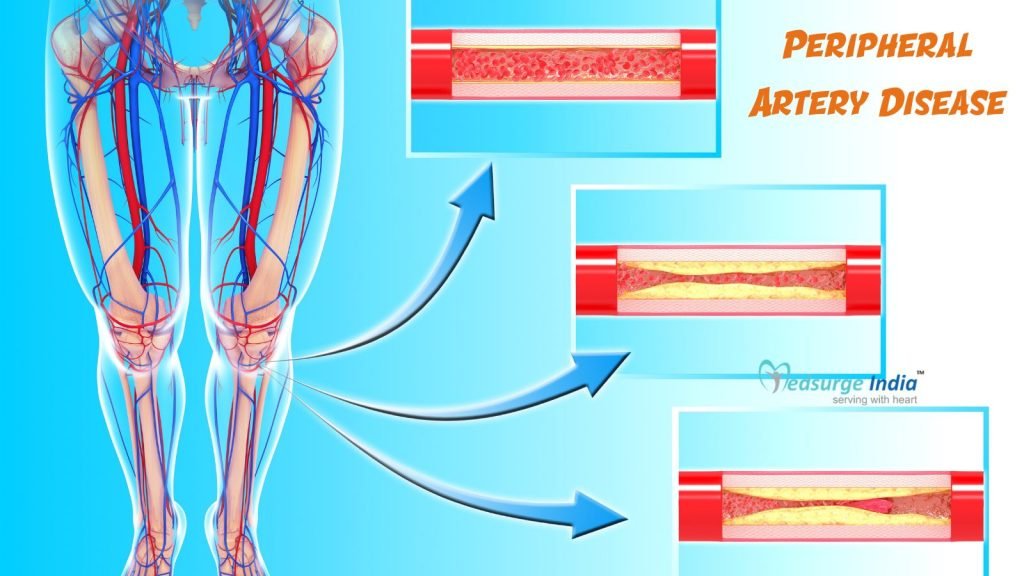
Diseases of the blood vessels beyond the heart and brain are referred to as peripheral artery disease (PAD). An accumulation of fatty deposits in the arteries is the most common cause. Peripheral arterial disease (PAD) is also known as a peripheral vascular disease (PVD) (which includes both arteries and veins).
PAD damages blood arteries, narrowing them and reducing blood flow to the arms, kidneys, stomach, and, most commonly, the legs.
Physical activity can significantly improve symptoms, despite the fact that the disease can have dangerous implications.
What Is Peripheral Artery Disease (PAD)?
Plaque buildup in the leg arteries that deliver oxygen and nutrient-rich blood from your heart to your arms and legs is known as a peripheral arterial disease (PAD), also known as peripheral vascular disease or peripheral artery disease.
A smooth lining avoids blood clotting and facilitates steady blood flow in arteries, which are shaped like hollow tubes. Plaque (composed of fat, cholesterol, and other substances) that accumulates gradually inside your arterial walls narrows your arteries when you have peripheral artery disease. Atherosclerosis is another name for this plaque.
The exterior of many plaque deposits is hard, while the inner is soft. Platelets (disc-shaped particles in your blood that help it clot) can come to the place where the hard surface cracks or tears, allowing them to clot. Blood clots can form around the plaque, narrowing the artery.
Blood can not get through to supply organs and other tissues if arteries become restricted or clogged by plaque or a blood clot. The tissues below the blockage suffer damage and finally die (gangrene). Your toes and feet are the most common places where this happens.
The rate at which PAD advances differs from individual to individual and is determined by a variety of factors, including the location of the plaque in your body and your overall health.
Peripheral Artery Disease Treatment Cost in India
The average cost of Peripheral Artery Disease Treatment in India can range from between 1200 USD to 3000 USD. It typically includes necessary preoperative tests, and the surgery itself. However, please note that accommodation and transfers are not included in this cost.
Types of Treatment For Peripheral Artery Disease Treatment in India
| Treatment | Starting Price |
| Peripheral Angioplasty | USD 1330 |
| Balloon Angioplasty | USD 2130 |
| Arterial Aneurysms | USD 4370 |
Note: Keep in mind that the aforementioned cost provided is solely for the treatment. The overall cost of Peripheral Artery Disease Treatment in India will be determined based on several factors.
Factors That Can Affect Peripheral Artery Disease Treatment Cost in India
Various factors can affect the cost of Peripheral Artery Disease Treatment in India. Your budget is greatly impacted by numerous elements that fail under pre and post-treatment costs. Below are the various factors that can affect the cost of Peripheral Artery Disease Treatment in India.
- Medication costs: Certain medicines can influence the overall cost of Peripheral Artery Disease Treatment.
- Patient Condition: The complexity of the disease along with the patient’s overall health can affect the duration of treatment, impacting the cost.
- Duration of treatment: Longer treatment courses involving multiple visits can lead to higher cumulative costs.
- Geographical location: Cost can vary widely depending on the region in India.
- Hospitalization expenses: The length of hospital stay and the level of nursing care required by the patient can add to the treatment expenses.
- Government policies and subsidies: Government healthcare schemes and subsidies can reduce out-of-pocket expenses for patients, affecting the affordability of Peripheral Artery Disease Treatment.
- Medical tourism packages: Curated packages for international patients can include various services at a bundled cost, influencing the overall expense of treatment in India.
- Hospital reputation and infrastructure: Prestigious hospitals with state-of-the-art facilities may charge more for their services.
- The expertise and experience of medical professionals: Cardiac surgeons with extensive experience and recognition often command higher fees, contributing to the treatment cost.
- The type and frequency of diagnostic procedures: Regular monitoring with advanced imaging and laboratory tests can increase treatment costs due to the high price of these diagnostic methods.
- The choice of treatment modality: Opting for newer or more advanced treatment options or precision medicine can be more expensive than traditional approaches.
Peripheral Artery Disease Treatment Cost in India offers exceptional medical services and facilities to patients who come for treatment in India also their facilities rival those of well-known healthcare centers worldwide. Accommodation, meals, and transportation expenses are also covered. Furthermore, a foreign patient can save up to 30-40% of the Peripheral Artery Disease Treatment cost in India when compared to their native countries.
What Are the Symptoms of Peripheral Artery Disease?
Many patients with peripheral artery disease have mild or no symptoms, although other people have leg pain when walking (claudication).
Claudication causes muscle soreness or cramping in your legs or arms that is induced by activity, such as walking but goes away after a few minutes of rest. The position of the clogged or narrowed artery determines the location of the pain. The most prevalent site of pain is the calf.
Claudication can range in severity from slight discomfort to immobilizing pain. You may find it difficult to walk or engage in other forms of physical activity if you have severe claudication.
The following are symptoms of peripheral artery disease:
- After certain activities, such as walking or ascending stairs, you may have painful cramping in one or both hips, thighs, or calf muscles.
- Numbness or weakness in the legs
- Coldness in your lower leg or foot, particularly on one side compared to the other
- Unhealing sores on your toes, feet, or legs
- The color of your legs has changed.
- On your feet and legs, you may notice hair loss or a slowing of hair development.
- Toenail growth will be slower.
- Legs with a lustrous sheen
- In your legs or feet, there is no or a feeble pulse.
- Men’s erectile dysfunction
- When stitching, writing, or doing other manual duties, you may have soreness and cramping in your arms.
What Are the Causes of Peripheral Artery Disease?
- Atherosclerosis is a common cause of peripheral artery disease. Atherosclerosis is a condition in which fatty deposits build up on the inside walls of your arteries, reducing blood flow.
- Although most people associate atherosclerosis with the heart, the disease can and often does affect arteries throughout the body. Peripheral artery disease happens when it affects the arteries that carry blood to your limbs.
- Blood vessel inflammation, injury to your limbs, the atypical structure of your ligaments or muscles, or radiation exposure is less prevalent causes of peripheral artery disease.
How Diagnosis of Peripheral Artery Disease Is Done?
Diagnosis of Peripheral Artery Disease can be done in a variety of methods, but if the disease is suspected, the doctor will first examine the patient’s legs.
The following are some of the tests your doctor may use to diagnose peripheral artery disease:
- Ankle-Brachial Index
- Blood testing, angiography, and ultrasound scan
- Doppler and duplex ultrasound imaging
- Angiography by computed tomography (CT)
- Magnetic Resonance Imaging (MRIA)
- Angiography
Peripheral Artery Disease that goes undiagnosed or untreated can lead to painful symptoms, loss of a limb, an increased risk of coronary artery disease, and carotid atherosclerosis (a narrowing of the arteries that supply blood to the brain).
Because persons with Peripheralartery disease have a higher risk of heart attack and stroke, experts advise people at risk to talk to their doctor about it so that it can be diagnosed and treated early.
Get Free Cost Estimation
Procedure
How to Cure Peripheral Artery Disease?
Peripheral artery disease treatment has two major goals:
- Manage symptoms like leg discomfort so you can get back to doing things you enjoy.
- Reduce your risk of heart attack and stroke by slowing the growth of atherosclerosis throughout your body.
You might be able to achieve these goals by making lifestyle modifications, especially if you are dealing with peripheral artery disease early on. Quitting smoking is the single most essential thing you can do to lower your risk of problems if you smoke. Walking or practising other forms of exercise on a regular basis, as part of supervised exercise instruction, can significantly improve your symptoms.
You will almost certainly require extra medical care if you have signs or symptoms of peripheral artery disease. Preventing blood clots, lowering blood pressure and cholesterol, and controlling pain and other symptoms are all things your doctor may recommend.
Medications
- Cholesterol-Lowering Medication
- High Blood-Pressure Medications
- Medication to Control Blood Sugar
- Medication to Prevent Blood Clots
- Symptoms-relief medications
In some circumstances, angioplasty or surgery may be required to treat claudication caused by peripheral arterial disease. Other prefered surgeries done to cure PAD are the following:
- Angioplasty
- Bypass Surgery
- Thrombolytic Therapy
To improve the distance you can walk painlessly, your doctor will most likely suggest a supervised exercise training programme. Regular activity helps your body use oxygen more efficiently, which improves Peripheral artery disease symptoms in a variety of ways.
Suggestion
Peripheral Artery Disease raises the risk of heart attack and stroke, therefore it’s critical to get it identified very away. Perspective is influenced by a variety of factors, however, following the lifestyle recommendations above can considerably improve your outlook.
Some cases of Peripheral artery disease can be treated with just a change in lifestyle and medicines.
The Most Important Frequently Asked Questions
Q: How Long Can You Live With Peripheral Vascular Disease?
A: If left undiagnosed and untreated, one in every five patients with PAD will have a heart attack, stroke, or die within five years. In addition to leg muscle pain, discomfort during activity, and loss of mobility and independence, untreated PAD can have other serious consequences.
Q: Is Peripheral Artery Disease a Death Sentence?
A: This disease is life-threatening and can lead to death. Lower-body peripheral artery disease is frequently a warning indicator. Other arteries, such as those that supply the heart or the brain, can accumulate plaque in a similar way.
Q: What Are the Stages of PAD?
A:
- Asymptomatic (Stage 0)
- Mild claudication (stage 1)
- Moderate claudication (stage 2)
- Severe claudication (stage 3)
- Pain relief (Stage 4)
Q: How Long Does PAD Surgery Take?
A: Your blood can now flow freely where it is needed, bypassing the barrier. You will not be awake for this surgery, which takes 2 to 5 hours. Typically, you will spend 3 to 7 days in the hospital.
Q: How Many Days Rest Are Needed After Angioplasty?
A: The average recovery period for angioplasty is two weeks, however, this can vary depending on your health. Stick to Your Medication Regimen: It’s critical to follow your medication schedule. Stopping your medicine too soon can put you at risk for a recurrence of cardiac condition.
Top Hospitals for Peripheral Artery Disease Treatment in India
Top Doctors for Vascular Surgery
Dr. Robbie George
Senior Consultant
Experience: 15 years of experience
University College of Medical Sciences, New Delhi
Bangalore, India
Dr. Suhail Naseem Bukhari
Director
Experience: 18 years of experience
BLK Super Speciality Hospital, New Delhi
New Delhi, India
Dr. Raghuram Sekhar
Consultant
Experience: 30 years of experience
Kokilaben Dhirubhai Ambani Hospital Mumbai
Mumbai, India
Dr. Vishal Sheth
Senior Consultant
Experience: 14+ years of experience
Narayana Multispeciality Hospital, Rakhial, Ahmedabad
Ahmedabad, India
Dr. Balaji V
Senior Consultant
Experience: 22 years of experience
Apollo Hospitals, Greams Road, Chennai
Chennai, India
Dr. Sunil Kumar Baranwal
Consultant
Experience: 11 years of experience
Fortis Hospital Delhi Shalimar Bagh
New Delhi, India
Dr. Sukalyan Purkayastha
Head of Department
Experience: 23 years of experience
Institute of Neurosciences, Kolkata
Kolkata, India
Dr. Amish Mhatre
Senior Consultant
Experience: 10 years of experience
Fortis Hospital, Mulund, Mumbai
Mumbai, India
Dr. P. Mohanty
Consultant
Experience: 43 years of experience
Batra Hospital & Medical Research Centre, New Delhi
NewDelhi, India
Dr. Rajiv Parakh
Chairman
Experience: 21 years of experience
Medanta – The Medicity, Gurgaon
Gurgaon, India
Dr. Jaisom Chopra
Senior Consultant
Experience: 35 years of experience
Indraprastha Apollo Hospital New Delhi
New Delhi, India
Dr. R Sekhar
Consultant , MBBS, MS, FRCS, FRCS
Experience: 13 years of experience
Kokilaben Dhirubhai Ambani Hospital, Mumbai
Mumbai, India
Dr. Azeez Pasha
Consultant
Experience: 20 years of experience
Manipal Hospital (Old Airport Road) Bangalore
Bangalore, India
Dr. Nitish Anchal
HOD
Experience: 19 years of experience
Indraprastha Apollo Hospital New Delhi
New Delhi, India
Dr. Tarun Grover
Senior Consultant
Experience: 21 years of experience
Medanta – The Medicity, Gurgaon
Gurgaon, India
Dr. Sumanth Raj KB
Consultant
Experience: 19 years of experience
Manipal Hospital Millers Road formerly Vikram Hospital Bangalore
Bangalore, India
Dr. N. Sekar
Vascular Surgeon Chief
Experience: 45 years of experience
Kauvery Hospital, Alwarpet, Chennai
Chennai, India
Dr. Rahul N.S
Consultant
Experience: 17 years of experience
Manipal Hospital (Old Airport Road) Bangalore
Bangalore, India
Dr. Kapil Mathur
Consultant
Experience: 20 years of experience
Apollo Specialty Hospital, OMR
Chennai, India