Beta Thalassemia: Types, Causes, Symptoms & Treatment
Reduced beta-globin production is a defining characteristic of beta-thalassemia. Since it is an inherited blood condition, at least one of your parents must be a carrier. Beta-thalassemia causes your body to create less hemoglobin than normal. Red blood cells that carry oxygen throughout the body include the iron molecule known as hemoglobin.
Healthcare professionals and doctors in India organize routine blood transfusions as part of beta-thalassemia treatment. The use of daily folic acid, iron-lowering drugs, bone marrow transplants, and other therapies is possible.
What is Beta- Thalassemia
A blood condition known as beta-thalassemia prevents your body from producing hemoglobin. Red blood cells are mostly composed of the iron-rich protein hemoglobin. Red blood cells transfer oxygen to other cells and tissues in your body thanks to hemoglobin. Your cells require oxygen for generating energy, which red blood cells give them.
Beta-thalassemia is one of the two primary types of thalassemia. Both beta-thalassemia and alpha-thalassemia are caused by gene mutations (or mistakes) in the hemoglobin protein. The production of beta-globin, a protein found in hemoglobin, is disrupted by this gene mutation.
What Are The Types of Beta- Thalassemia
The severity of your ailment will depend on the number of faulty genes you inherit as well as the location of the mutation. Some mutations result in the production of no beta-globin (beta-zero thalassemia). Other mutations result in the production of too little beta-globin (beta-plus thalassemia).
The following are examples of beta thalassemia types.
- The most severe form of beta thalassemia is beta thalassemia major, often known as Cooley’s anemia. Two beta-globin genes are either absent or broken in this condition. Because individuals with beta-thalassemia major require ongoing blood transfusions, the disorder is now referred to as “transfusion-dependent thalassemia”.
- Mild to moderate anemia symptoms could be brought on by beta thalassemia intermedia. Two beta-globin genes must also be absent or damaged. With beta thalassemia intermedia, you most likely won’t require lifelong blood transfusions.
- Mild anemia symptoms are frequently brought on by beta thalassemia minor (beta thalassemia trait). One beta-globin gene is either missing or damaged in this condition. The symptoms of beta thalassemia minor can be completely absent in certain people.
How Does Beta-Thalassemia Affect The Body
Your red blood cells suffer damage as a result of low beta-globin production, which causes them to stop moving through the bloodstream. Anaemia sets in if your body is unable to produce enough new red blood cells to replace the ones that are lost. Anaemia symptoms appear when there are insufficient red blood cells to transfer oxygen to your body’s tissues, depriving them of oxygen.
The severity of beta thalassemia-related anemia symptoms depends on how low your red blood cell count is.
Risk of Beta-Thalassemia
It is possible to inherit beta thalassemia from one parent or from both parents as a genetic condition. Having a family history of the disease is the only risk factor that can increase your risk of contracting the disease.
What Causes Beta-Thalassemia
A mutation (error) that restricts the body’s ability to produce beta-globin leads to beta-thalassemia. Two alpha-globin chains and two beta-globin chains make up the four protein chains that make up hemoglobin. Alpha thalassemia is brought on by mutations in the alpha-globin chain, whereas beta thalassemia is brought on by mutations in the beta-globin chain. The red blood cell is harmed and eventually destroyed when either globin chain is lacking.
The beta thalassemia gene mutation is inherited in an autosomal recessive manner. This occurs when one copy of the mutant gene and one copy of the normal gene are present in each of the two biological parents. You receive a copy of the mutated gene from both parents if you have the most severe form of beta-thalassemia. Rarely, beta thalassemia is brought on by inheriting a single defective beta-globin gene. An autosomal dominant pattern is what this is.
Read about Thalassemia Treatment Cost in India.
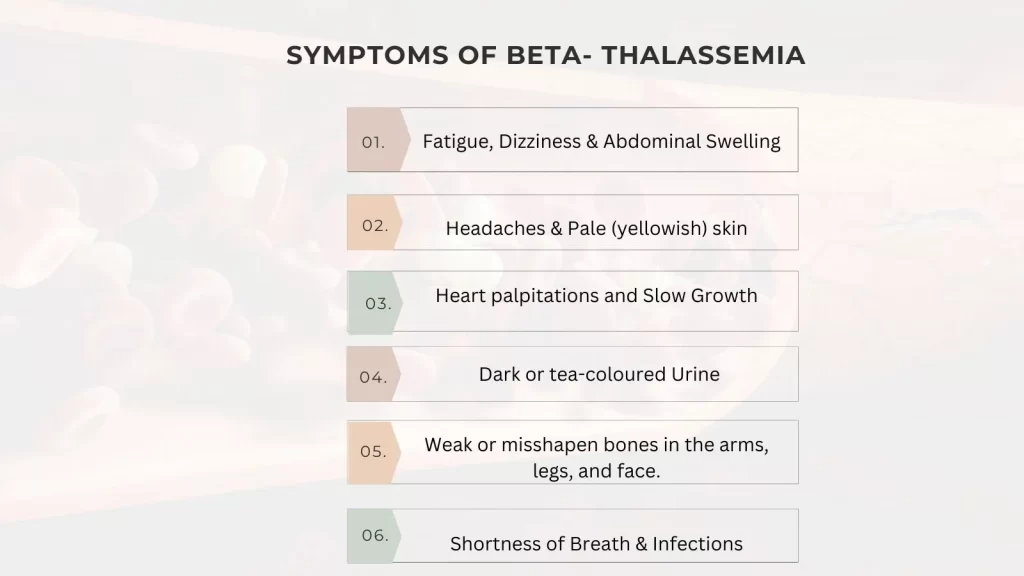
What Are The Symptoms of Beta- Thalassemia
Your symptoms will depend on the degree of beta-thalassemia in your body. You can experience no symptoms at all or only mild anemia symptoms if you have a beta-thalassemia minor. Beta-thalassemia major, in particular, can result in symptoms that range from moderate to severe. The following list of beta-thalassemia signs and symptoms:
- Fatigue
- Dizziness
- Headaches on a regular basis
- Pale (yellowish) skin
- Shortness of breath
- Heart palpitations
- Symptoms of jaundice
- Dark or tea-colored urine
- Slow growth
- Abdomen swelling
- Weak or misshapen bones in the arms, legs, and face.
- Infants that have moderate to severe beta-thalassemia may get infections on a frequent basis.
Signs and symptoms of thalassemia intermedia can appear in early childhood or later in life. Depending on the specific kind of mutation, the disease’s severity can change. For more info read about Beta-Thalassemia Treatment Cost in India.
How is Beta-Thalassemia Diagnosed
Children are frequently the first to be diagnosed with beta-thalassemia. By the age of 2, beta thalassemia major, the most serious variant, is identified. Based on your symptoms and the findings of a blood test, your doctor will determine whether you have beta-thalassemia.
1. A complete blood count (CBC) test provides information about your white and red blood cells. The test identifies whether your red blood cells are too few, smaller, abnormally shaped, or pale.
2. Reticulocyte count: Reticulocytes, or immature red blood cells, are counted. Your body is not making enough red blood cells if your reticulocyte count is low. Additionally, this may result in severe health issues like anemia, liver, bone marrow, and other illnesses.
3. Molecular genetic testing enables the physician to closely study the hemoglobin and pinpoint the mutation responsible for beta-thalassemia by detecting changes in a single gene as well as huge duplications or depletions.
4. Haemoglobin electrophoresis: This test measures several hemoglobin protein types and gives medical professionals a general picture of the situation.
During pregnancy, the doctor may undertake chorionic villus sampling (CVS) or amniocentesis if there are any worries that the fetus may carry the mutant gene. The organs and organ systems of a person with beta-thalassemia may need to undergo further, continuing testing.
Helpful information, Alpha Thalassemia Treatment Cost in India.
How is Beta- Thalassemia Treated
Since beta-thalassemia has no known treatments. Treatment for beta-thalassemia is based on the disorder’s severity and type of symptoms. Options for treatment include:
Blood transfusions may be necessary as frequently as every two weeks for those with beta-thalassemia major. During this treatment, a patient will get blood from a donor.
Chelation therapy for iron: Iron is a crucial part of hemoglobin, which enables it to carry oxygen. On the other side, too much iron might be dangerous. To avoid iron excess, iron chelation therapy is done.
Supplemental folic acid: Folic acid enhances the body’s capacity to create red blood cells. Your doctor could suggest taking vitamins if you have beta thalassemia mild. Your doctor could advise taking folic acid in addition to getting regular blood transfusions if your problem is severe.
Luspatercept: To encourage the body to manufacture more red blood cells, patients with severe thalassemia may receive injections of Luspatercept every three weeks. When beta-thalassemia patients receive blood transfusions, lupatercept frequently reduces anemia.
Transplantation of bone marrow and stem cells: Patients may receive bone marrow stem cells from donors. Beta-thalassemia can be cured by switching out the bone marrow stem cells with healthy donor stem cells.
A bone marrow and stem cell transplant from a suitable donor is the treatment option for beta-thalassemia.
Who Can Be The Donor
- Matched Family donor is the best option. A matched family member who has Thalassemia trait can also be a donor for a patient with Thalassemia major.
- Matched Unrelated Donor from World Wide Registries can also be considered for BMT.
- HAPLOIDENTICAL (Half Matched) FAMILY DONOR might be a viable option for the patients who do not have matching donor.
Ref. website – https://www.bloodsrus.com/terms/thalassemia-and-related-disorders/5448
Best Hospitals for Beta Thalassemia Treatment in India
- Fortis Hospital Gurgaon
- Medanta Hospital, Gurgaon
- Artemis Hospital Gurgaon
- Manipal Hospital Dwarka, Delhi
- Fortis Hospital Noida
- Amrita Hospital, Faridabad
- Global Hospital Mumbai
- Apollo Hospitals, Greams Road, Chennai
- Kauvery Hospital, Chennai
Bottom Line
Depending on how serious your illness is, how you respond to beta thalassemia will vary. Working with experts who have experience detecting and treating thalassemia is crucial, regardless of the kind of beta-thalassemia. Getting the proper care can lower your risk of issues like iron overload and help prevent anemia. Your prognosis can be improved by collaborating with a care team that will monitor your status suitably and offers a personalized treatment plan.