Cutaneous infiltration of malignant monoclonal T cells is a characteristic of the diverse group of extranodal non-lymphomas Hodgkin’s known as cutaneous T cell lymphomas (CTCLs). The frequency is around 0.5 per 100,000 people per year, and they generally affect adults with a median age of 55 to 60 years. The three most significant subtypes of CTCL are primary cutaneous peripheral T cell lymphomas that are not otherwise defined, Sézary syndrome, and mycosis fungoides. The etiopathogenesis, diagnosis, treatment, and prognosis of CTCL are complex concepts. Medical professionals in India treat Cutaneous T-Cell Lymphoma in various ways. The major forms of treatment are drugs, radiation therapy, light therapy, etc.; if necessary, a patient may even have a stem cell transplant. Your doctor can suggest using natural therapies like using mild, unscented soap and keeping yourself hydrated.
In India, the cost of treating Cutaneous T-Cell Lymphoma is affordable when compared to that of other industrialized countries. The skill of hematologists/oncologists, and the state-of-the-art medical equipment used at the top Indian hospitals may be partially credited for the success. In addition to these advantages, India is well known for its low costs without lowering clinical standards.
What is Cutaneous T-Cell Lymphoma?
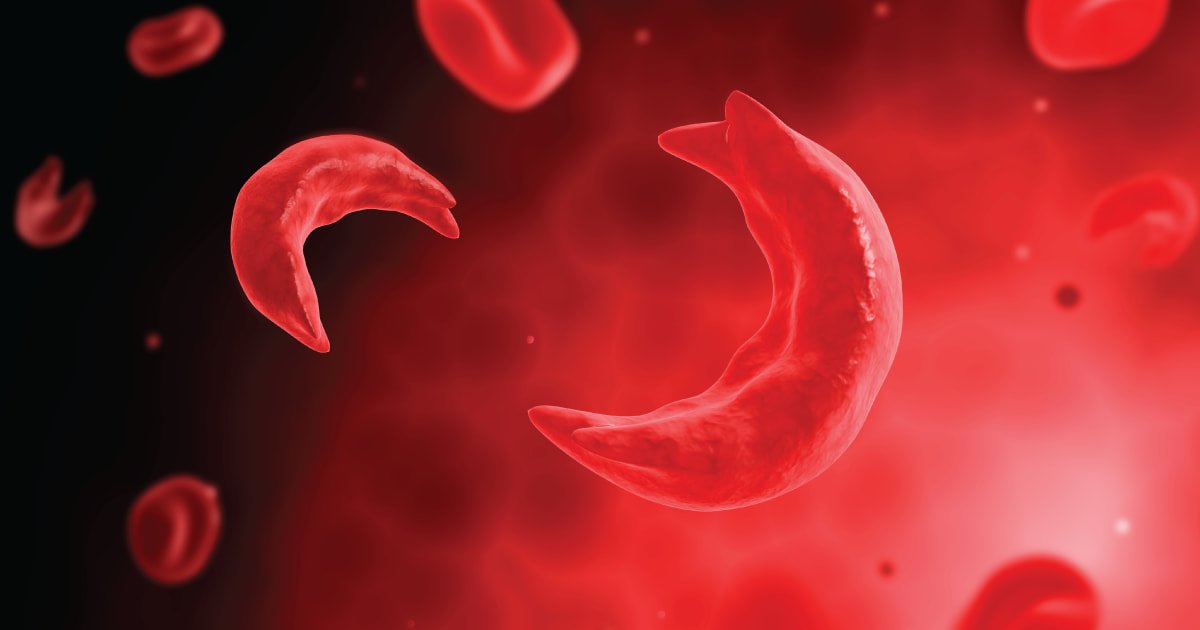
Cutaneous T-cell lymphoma is a class of uncommon blood malignancies that affects the skin, which is the biggest organ in the body. These malignancies can present with signs that resemble common skin conditions, such as rash, very itchy skin (pruritus), or other skin problems. Although most cutaneous T-cell lymphomas are non-lethal and grow extremely slowly, certain individuals may have more severe manifestations of the disease. Medical professionals can treat symptoms, but they cannot treat lymphomas.
Cutaneous T-cell lymphoma often progresses slowly. It takes several years to develop. The Sezary syndrome and mycosis fungoides are the 2 most prevalent subtypes of this malignancy.
What are the Signs and Symptoms of Cutaneous T-Cell Lymphoma?
Depending on how far the malignancy has gone, cutaneous T-cell lymphoma symptoms vary. The signs may resemble those of other skin disorders. Do not hesitate to consult your doctor if you receive a diagnosis. The followings are the most typical mycosis fungoides and Sezary syndrome signs and symptoms:
- Itchy, round areas of skin that may be elevated or scaly
- Skin patches that contrast with the surrounding skin in colour
- Lumps that develop on the skin and may become visible
- An increase in lymph nodes
- hair fall
- The skin on the palms of the hands and the soles of the feet become thicker
- A very irritating, rash-like skin redness that covers the whole body.
What Causes Cutaneous T-Cell Lymphoma?
It is unknown what specifically causes cutaneous T-cell lymphoma. Cancer often starts when cells’ DNA undergoes alterations (mutations). The DNA of a cell carries instructions that direct the cell’s actions. The DNA changes to instruct the cells to expand and divide quickly, producing a large number of aberrant cells.
The mutations in cutaneous T-cell lymphoma lead to an excess of aberrant T cells that assault the skin. Your immune system includes T cells, which typically assist your body in battling pathogens. The reason the cells assault the skin is unknown but doctors believe it may be due to two reasons which are as follows;
- Acquired genetic mutations: Scientists have identified several gene alterations that result in these diseases. They are currently investigating why specific genes alter.
- Infections: When you have an infection, your immune system kicks into overdrive. In response, your bone marrow produces more lymphocytes more quickly. Similar to any manufacturing line, a procedure that is sped up could result in errors. In this instance, the errors result from DNA mutations that impact crucial genes in cells and ultimately lead to lymphoma. Researchers are looking at any connections between cutaneous T-cell lymphoma and infections.
How is Cutaneous T-Cell Lymphoma Diagnosed?
In order to identify cutaneous T-cell lymphoma, the following tests and techniques are used:
- Physical examination: Your doctor will look for firm, elevated growths or patchy, scaly areas on your skin. Additionally, your organs and lymph nodes will be checked for any indications that you could have an issue.
- Blood tests: The total blood count and other blood tests may be done to better understand your situation. Blood tests can occasionally reveal cancer cells, especially in cases with Sezary syndrome.
- Biopsies: In order to make a diagnosis, medical professionals take samples of the skin. To correctly identify cutaneous T-cell lymphoma, they might need to do many skin samples. They could also take samples of your lymph nodes and any other areas of your body that cutaneous T-cell lymphoma might affect.
- Imaging tests: Your doctor may suggest imaging tests like computed tomography (CT) or positron emission tomography (PET) scans if there is the worry that the cancer cells have moved to other areas of the body.
Get Free Cost Estimation
Procedure
How Cutaneous T-Cell Lymphoma is Treated?
Skinny T-cell lymphoma patients have access to a wide range of therapies. The optimal course of therapy for you will depend on your unique circumstances, including the severity or stage of your lymphoma. For cutaneous T-cell lymphoma, the majority of patients get a combination of therapies.
Treatment choices might be:
- Extracorporeal photophoresis (ECP): This procedure uses psoralen and UV light. White blood cells are extracted from your blood by the providers. They combine psoralen with those cells. UV radiation can now damage malignant cells as a result. The cancer cells are subsequently killed when these cells are exposed to UV radiation. The modified white blood cells are then returned to your circulation.
- Phototherapy: This treatment is employed in the early stages of illness. In phototherapy, medical professionals treat early-stage illness using ultraviolet A (UV-A) or B (UV-B) light. They could do a PUVA therapy, which combines UV-A and psoralen. After taking the drug, medical professionals expose the skin’s afflicted regions to UV radiation. The drug is activated by light, which also destroys cancer cells.
- Radiation treatment: Energy beams are used in radiation treatment to eliminate cancer cells. It may be advised to use normal radiation therapy with X-rays if you just have one region of cutaneous T-cell lymphoma. Electron beam radiation treatment, which targets the skin and spares internal organs, may be used for patients with more extensive cancer. The whole skin is often exposed to electron beam radiation.
- Medications: Medications used to treat cutaneous T-cell lymphoma include immune system suppressants such as interferon and steroid medications. Chemotherapy drugs target cancer cells and other rapidly proliferating cells. The unique vulnerabilities of cancer cells are the focus of drugs used in targeted treatment.
- Immunotherapy: This procedure uses your body’s natural compounds or those created in a lab to strengthen your immune system. Immunotherapy aids in the reduction or elimination of cancer cells.
- Chemotherapy: You can use gels, creams, or lotions directly on the damaged parts of your skin, take chemotherapy tablets orally, intravenously (IV), or both.
- Skin ointments and creams: Creams, gels, and ointments are all forms of medications that can be administered topically to the skin. An anti-itching and anti-redness medication such as corticosteroids can reduce itching and skin redness. To combat cancer cells, chemotherapy can be given topically to the skin.
- Bone marrow transplant: The process of replacing your unhealthy bone marrow with healthy bone marrow from a matched donor is known as a bone marrow transplant, also known as a stem cell transplant (allogeneic bone marrow transplant). You’ll be given chemotherapy medications during the transplant to suppress your sick bone marrow. After that, your body is filled with healthy donor cells, which go to your bones and start repairing your bone marrow.
What is the Cost of Cutaneous T-Cell Lymphoma Treatment in India?
Comparatively speaking to other nations, India has far cheaper healthcare prices. Additionally, the level of medical care and services offered there are on par with those at the greatest hospitals in the world. Even without factoring in the costs of travel, hotel, and food, the cost of Cutaneous T-Cell Lymphoma Treatment in India starts from USD 4500.
In India, the total cost of Cutaneous T-Cell Lymphoma Treatment might vary based on a variety of factors, including
- Depending on the hospital’s preferences, the cost of treatment packages may vary.
- The doctor’s knowledge and expertise in the area.
- The situation of the patient: The patient’s illness and whether additional treatment modalities are necessary for complete care.
- Hospitalization and travel time in the nation.
- Post-operative care is required.
- categorization of a hospital room.
How to Choose a Hospital in India for Cutaneous T-Cell Lymphoma Treatment?
Hospitals that treat Cutaneous T-Cell Lymphoma are widely renowned for their patient care and hospitality offerings. These facilities are home to some of India’s top oncologists, dermatologists, and experts in their areas. It could be challenging for a foreign patient to select a reputed hospital for treatment. It is an important choice that needs to be made while keeping a number of things in mind, like:
- Accreditations and certifications for excellence
- Location of the hospital and the transit hub
- The medical and surgical staff
- Modern diagnostic and treatment tools
- Overseas medical help
How can Medsurge India Help?
Medsurge India is a prestigious support system for patients looking for doctors, hospitals, and specialized treatments. We’ll find the most suitable medical options for you. Regarding your medical issues, our team will give you a list of certified, reputable, and trusted doctors and hospitals. Additionally, we offer a treatment strategy that fits your budget. Apart, we assist patients with obtaining travel authorizations, medical visas, and a multitude of other things.
The Most Important Frequently Asked Questions
Q1: Which therapy is most effective for T cell lymphoma?
A1: The most common kind of treatment is intense chemotherapy using numerous medications. The chemotherapy employed is frequently CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone). Radiation treatment may also be utilised if the lymphoma is isolated to a single region.
Q2: Is it possible for cutaneous T-cell lymphoma to spread?
A2: In addition to the lymph nodes and other organs, this cancer can move from the skin to the blood. Chemotherapy, radiation, and photodynamic therapy are all possible forms of treatment.
Q3: What stage of T cell lymphoma is considered advanced?
A3: Stages IIB through IVB are regarded as severe stages of the illness, when the cancer has spread to other areas of the body or has left the skin to affect other organs or lymph nodes.
Q4: Which type of lymphoma is worse, B-cell or T-cell?
A4: Except for individuals with low-grade histology, the median survival duration for patients with Stage III and IV lymphomas was nine months for T-cell lymphomas and 17 months for B-cell lymphomas. It was discovered that T-cell lymphomas had a much worse prognosis than B-cell lymphomas.
Q5: Is it possible to misdiagnose T-cell lymphoma?
A5: Due to the nonspecific clinical and pathologic characteristics of angioimmunoblastic T-cell lymphoma (AITL), it is typical for it to be misdiagnosed as another kind of lymphoma. Dermatologists and dermatopathologists can be crucial in the identification of this challenging cancer.
Top Hospitals for Cutaneous T-Cell Lymphoma Treatment in India
Top Doctors for Oncology and Oncosurgery
Dr. Ankur Bahl
Director
Experience: 14 years of experience
Fortis Memorial Research Institute, Gurgaon
Gurgaon, India
Dr. P. Rajkumar
Consultant
Experience: 23 years of experience
Apollo Cancer Hospital, Chennai
Chennai, India
Dr. Vaibhava Srivastava
Consultant
Experience: 9 years of experience
Apollo Medics Super Speciality Hospital, Lucknow
Lucknow, India
Dr. Gunjan Baijal
Experience: 20+ years of experience
Manipal Hospital, Panaji, North Goa
North Goa, India
Dr. Mansi Khanderia
Consultant
Experience: 8 years of experience
SS SPARSH Hospital (Mysore Road) Bangalore
Bangalore, India
Dr. N. Kathiresan
Consultant
Experience: 24 years of experience
Dr. Kamakshi Memorial Hospital Chennai
Chennai, India
Dr. Kumara Swamy
Senior Consultant
Experience: 36 years of experience
Aster CMI Hospital (Hebbel) Bangalore
Bangalore, India
Dr. Mandeep Singh Malhotra
Senior Consultant
Experience: 15 years of experience
Fortis Memorial Research Institute, Gurgaon
Gurgaon, Haryana
Dr. Sabyasachi bal
Chairman
Experience: 34 years of experience
Sir Ganga Ram Hospital, New Delhi
New Delhi, India